Type 1 diabetes is a life-long autoimmune disease characterized by the body’s inability to produce sufficient insulin. With Type 1 diabetes, the pancreas stops producing insulin, causing a dangerous build-up of sugar in the blood. Left untreated, this can be fatal. While the cause of Type 1 diabetes is still unknown, research suggests it is caused by both genetic and environmental factors.

Common symptoms of Type 1 diabetes can include excessive thirst, frequent urges to urinate, feeling tired throughout the day, and rapid weight loss. Type 1 diabetes is a serious condition that can have a severe impact on individuals’ quality of life. However, the current treatments available are limited in effectiveness and come with numerous drawbacks, meaning that more effective treatments are urgently needed.
As such, the medical community must work together to develop better solutions that can reduce the impacts of Type 1 diabetes and increase the overall well-being of those living with this condition. Research into existing treatments as well as completely new approaches could be beneficial in helping identify potential treatments that offer improved support for patients with Type 1 diabetes.
Stem cell therapy for Type 1 diabetes is a promising new treatment that has the potential to significantly improve patient outcomes. By introducing healthy insulin-producing beta cells into the body, this treatment may potentially reduce or even eliminate many of the complications that are present with Type 1 diabetes, such as heart disease and blindness.
While further research is needed in order to fully understand the efficacy of stem cell therapy for this condition, initial studies have demonstrated its effectiveness in both pre-clinical and clinical settings. The development of stem cell therapies for Type 1 diabetes has been groundbreaking, offering hope to those who previously had none available.
A study, Implanted pluripotent stem-cell-derived pancreatic endoderm cells secrete glucose-responsive C-peptide in patients with type 1 diabetes, is looking into how stem cells can improve type 1 diabetes outcomes.

Results of the Study
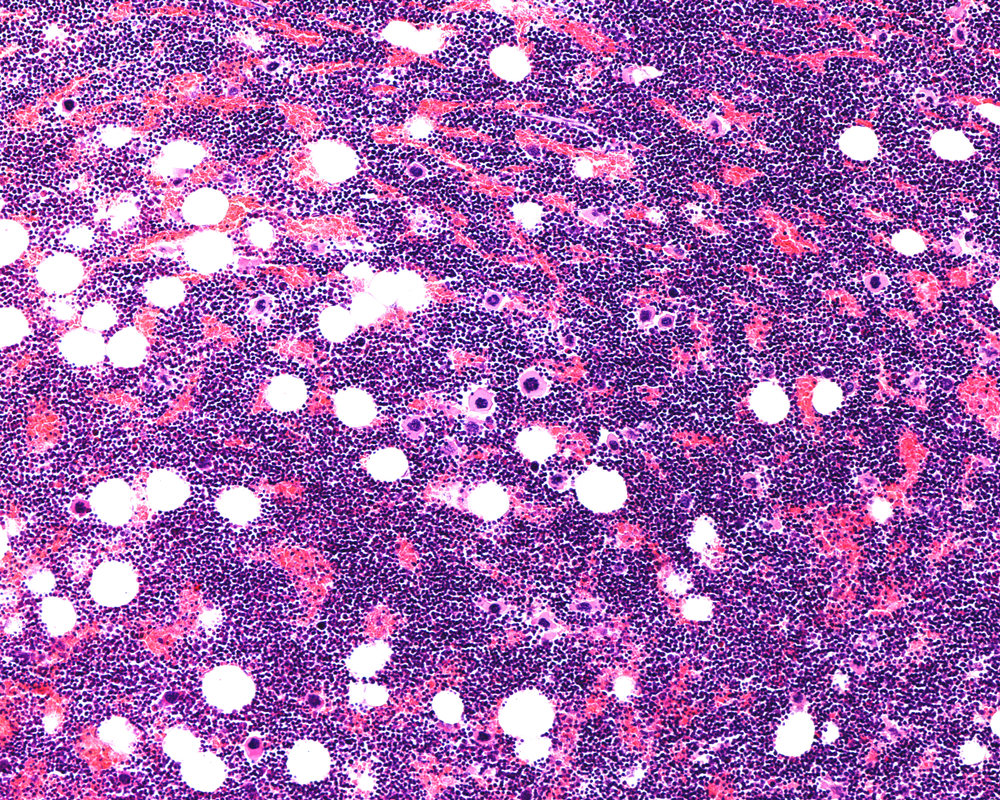
Researchers conducted a study to assess the efficacy and safety of pancreatic endoderm cells (PECs) that were implanted in microencapsulation devices as a potential treatment for type 1 diabetes. Patients received 250–500 million PEC-01s that were delivered via a pouch implanted under the skin on the backs of patients. There were 15 patients involved in the study. The patients had been diagnosed for at least five years and did not have the ability to tell when their blood sugar went too low.
The hope is that the stem cells will differentiate into insulin-producing pancreatic islet cells. Analysis of one year of data from 15 patients revealed that subcutaneous implantation of these cell products combined with immunosuppression was well tolerated, without any teratoma formation or severe graft-related adverse events.
Patients developed mixed meal-stimulated C-peptide secretion and experienced increased fasting C-peptide levels and glucose-responsive C-peptide levels. Immunosuppression also resulted in transient increases in circulating regulatory T cells, PD1 high T cells, and IL17A+CD4+ T cells.
There was an increase in C-peptides after meals which pointed to the successful boosting of insulin production by the implanted cells. Data showed that patients experienced a decrease in HbA1C, an average of 1.5%, as well as a reduction in insulin doses by up to 70%.
This data represents a breakthrough in science as it is the first reported evidence of differentiated stem cells producing meal-regulated insulin secretion. The progress has brought new hope to those with Type 1 Diabetes and treated patients spent 13% more time within the target range for their blood sugar levels.
Even better, some managed to reduce the amount of insulin they had been injecting prior to treatment. It is hoped that this revolutionary technique will help people with T1D improve their health outcomes and eventually free them from depending on insulin injections every day.
This study suggests that PEC-Direct holds promise as a potential functional cure for type 1 diabetes; one which eliminates the need for external dosing or injections. The study further highlights the importance of continually optimizing this treatment as it has the power to revolutionize life for those affected by type 1 diabetes.