Without enough food, no human could live for more than a few weeks. But access to healthy foods won’t keep you in good health if your gastrointestinal system can’t extract the vital nutrients, vitamins, and energy you need to survive, let alone thrive.
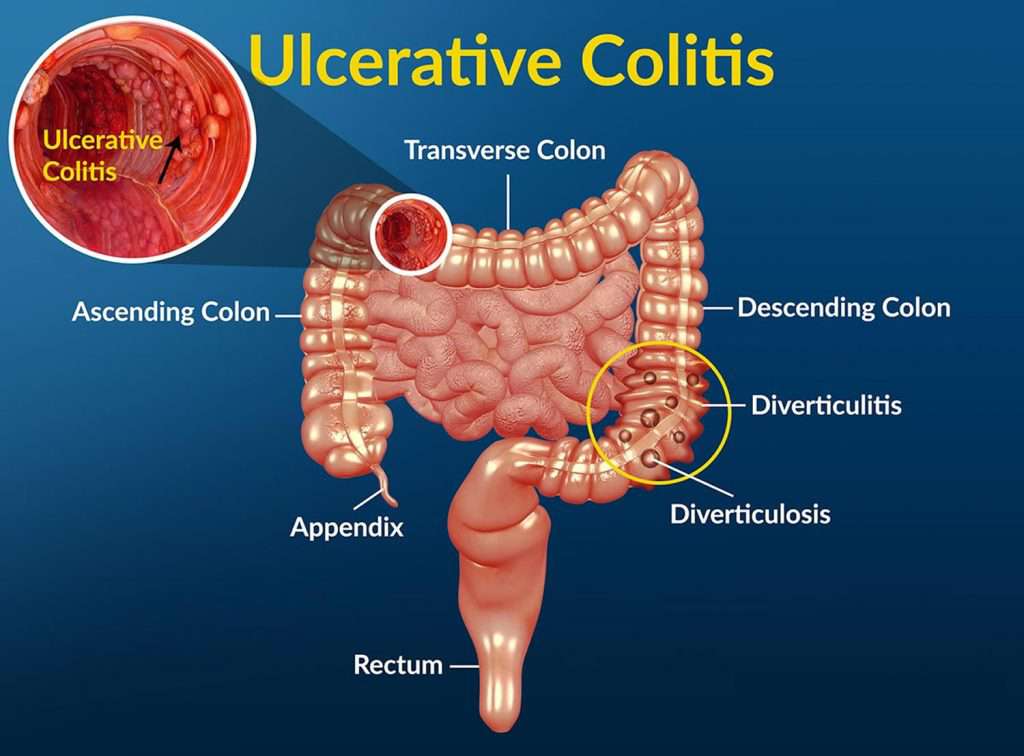
Indeed, any disorder that interferes with digestion can cause illness, pain, or even death. One disease that can disrupt normal digestive processes is ulcerative colitis. Although the gastrointestinal tract extends from the mouth all the way down to the stomach, intestines, and rectum, ulcerative colitis affects a specific part of the digestive tract – the large intestine (colon) and rectum.
In the United States, about one million people suffer from ulcerative colitis, which can be a disease that makes life miserable. Not only does it cause severe symptoms, but these symptoms can also fluctuate in severity in an unpredictable way. Patients never know when symptoms such as sudden bouts of bloody diarrhea and abdominal pain may flare up, nor when they will ease again – or even get worse. This disease may become so serious that patients need to be hospitalized for treatment or even undergo surgery.
Unfortunately, current treatment options can only alleviate symptoms because there is no cure for ulcerative colitis. But ongoing research into stem cell therapy shows that these advanced treatments may offer more hope to those who suffer from this disease. Some evidence suggests that stem cells may hold the key to developing a cure, or work better than current treatment options to help make symptoms less severe and less frequent.
One reason that stem cell therapy seems to a promising approach to treatment is that ulcerative colitis is an inflammatory disease and stem cells are known to help control inflammation caused by other disorders. Understanding the nature of this disease shows how stem cells may help patients suffer fewer symptoms and, in some cases, avoid the need for surgery.
What is ulcerative colitis? An inflammatory bowel disease
As a disease that’s classified as inflammatory bowel disease, ulcerative colitis causes inflammation and ulcers that are generally confined to the colon and rectum but can extend into other parts of the digestive system in some cases. It’s usually a long-term condition that emerges gradually over time, not a disease that comes on suddenly.
Scientists believe that the inflammation that ulcerative colitis causes are the result of a poorly functioning immune system. The body’s immune system is designed to attack microbes and other pathogens that cause disease. In some cases, however, the immune system misidentifies food as a threat to health and signals white blood cells to move into the colon and rectum to attack and fight off these “foreign invaders.” When the immune system functions normally, these attacks help defend us against disease, but too many white blood cells in the colon and rectum that aren’t fighting disease at all can cause inflammation, pain, and the formation of ulcers.
Symptoms may range from mild to severe and can fluctuate over time. These symptoms include:
- Abdominal pain from inflammation in the colon and rectum
- Weight loss, in part from a poor appetite
- Diarrhea that may include blood
- Fatigue
- Fever
- Malnutrition and dehydration
The severity and frequency of symptoms may be based on several factors including age and diet. Nearly half of patients (45 percent) do not report symptoms, but lab tests will show inflammation is present in the colon and rectum.
There are several types of this disease that affect various parts of the digestive system, including:
- Ulcerative proctitis: Generally a less severe form of this disease that causes inflammation only in the rectum, ulcerative proctitis can cause rectal bleeding so it may remain undiagnosed if symptoms are mild.
- Proctosigmoiditis: This form of ulcerative colitis can cause more symptoms than ulcerative proctitis and affects both the rectum and lower end of the colon. Symptoms include bloody diarrhea, pains, and cramps. Patients also report needing to use the bathroom but are unable to do so.
- Left-sided colitis: This form of the disease causes inflammation that extends from the rectum all the way up to the descending colon on the left side of the body. This is why symptoms in this form of the disease are generally felt on that side of the abdomen and can be even more severe.
- Pancolitis: This is the most serious type of ulcerative colitis because it affects the entire colon and rectum. Symptoms can be very severe and include bloody diarrhea, fatigue, pain, and weight loss. Thankfully, this is the least common type of ulcerative colitis.
Increased risk of cancer
Patients with ulcerative colitis face a higher risk of developing colon cancer. Some researchers believe that the inflammation from this disease can cause the cells in the lining of the colon to become cancerous. Studies suggest that the longer a patient suffers from this disease, the more likely it is that cancer may develop.
A study in 2012 showed that patients with ulcerative colitis are more likely to develop colon cancer compared to patients without the condition. A 2008 review of long-term patients with ulcerative colitis demonstrated how that risk grows over time after they are diagnosed with the disease:
- 2% risk after 10 years
- 8% risk after 20 years
- 18% risk after 30 years
Comparing this data to the incidence of colon cancer in the general population – less than 5 percent overall – demonstrates why it’s so important that patients get effective treatment. It also shows why stem cell therapy may help patients not only suffer fewer symptoms but prevent the incidence of more serious illnesses in the future.
What causes ulcerative colitis?
Researchers have not yet been able to provide any conclusive cause for ulcerative colitis because the underlying mechanisms aren’t clearly understood – and there may be several factors that contribute to the emergence of this disease. This makes developing treatments more complex.
One factor that seems to be associated with ulcerative colitis is that it seems to be more commonly diagnosed in more developed and industrialized countries compared to other parts of the world. Some researchers believe that in the developed world, resistance to infectious microbes may be less. Data also suggest that levels of sulfate-reducing bacteria are generally higher in patients with ulcerative colitis, which can increase levels of hydrogen sulfide in the colon and lead to symptoms of the disease.
Another theory is that the disease may be caused by infection with a bacterium called mycobacterium avium, one that the immune system may not be able to resist with enough strength to fight off infection and thus lead to ulcerative colitis.
Other research suggests that ulcerative colitis could be based on a poorly functioning immune system, which as noted earlier can lead to excess inflammation when too many white blood cells enter the colon and rectum.
Risk factors that seem to be associated with cases of ulcerative colitis include:
- Genetics: Family history can be a factor in the development of this disease. If one family member is diagnosed with ulcerative colitis, it is more likely that another member of the family will also be diagnosed with this disease. In fact, researchers have identified specific genes that may be associated with ulcerative colitis.
- Ethnic background: Patients with an Anglo-Saxon background are more likely to develop the disease rather than Asian, black, or Latinx communities. Researchers are not entirely sure why ethnic background may be a factor in the risk of developing ulcerative colitis, but data suggests there may be a relationship.
- Environment: Various environmental factors seem to be associated with this disease. For example, those who have been breastfed as an infant are less likely to suffer from ulcerative colitis than those who were not. And although the evidence remains inconclusive, some research shows that while a diet high in fats may not be a factor in developing this disease, it may result in symptoms that are more severe.
- Age Because ulcerative colitis emerges slowly over time, younger people do not usually experience symptoms. In fact, most cases are generally diagnosed in patients over the age of 30, and less commonly diagnosed before that age.
It’s important to note that ulcerative colitis is only one type of inflammatory bowel disease. Another type, one less commonly diagnosed, is called Crohn’s disease.
The right diagnosis:
The difference between ulcerative colitis And Crohn’s disease
Many patients we talk to are often confused by another similar disease that causes similar symptoms, but is a different disorder — Crohn’s disease.
It’s important to understand the difference because treatments can vary and a misdiagnosis could lead to less effective treatment.
Ulcerative colitis is three times more prevalent than Crohn’s disease. The main difference between the two is that while ulcerative colitis is usually confined to the colon and rectum, Crohn’s disease can affect areas higher in the digestive tract. Also, Crohn’s disease can affect the skin, eyes, joints, and liver, which can cause additional symptoms that make managing the disease even more complex.
Another difference between these two diseases is the location of the inflammation that develops. Ulcerative colitis tends to affect only the innermost layer of the colon, while Crohn’s disease can inflame all layers of the bowel wall.
While Crohn’s disease typically causes more severe symptoms than ulcerative colitis, more patients with ulcerative colitis undergo surgery than those with Crohn’s disease.
Current treatments for ulcerative colitis
The medical community has developed a number of treatments for ulcerative colitis. There is not yet a cure for ulcerative colitis, so the focus of treatment is on managing the symptoms so they are less severe and when symptoms ease, keeping the disease in remission for as long as possible. Current treatments include:
Medications
This is one of the first treatment options that physicians consider, although medications may not always be effective. One medication may not be enough to manage symptoms, so for many patients, a second medication may be needed. Commonly prescribed medications include:
- Anti-inflammatory medications: These may be effective in helping patients with mild cases of ulcerative colitis. Examples include Azulfidine, Asacol HD, Delzico, Colazal, and Dipentum. But these medications can cause side effects, so they are not usually used for long-term treatment.
- Immune system suppressors: If anti-inflammatory medications aren’t effective, physicians may prescribe these medications to control the body’s immune response. Unfortunately, using these medications can reduce the body’s defenses against other pathogens and make patients even more susceptible to other infections. Other side effects include liver and pancreas problems, blood clots, and a higher risk of the incidence of shingles.
- Biologics: These medications target proteins produced by the immune system to neutralize specific proteins that can cause inflammation. One such medication, tofacitinib, was approved by the FDA in 2018. This medication is typically used for patients with moderate to severe ulcerative colitis.
Lifestyle changes
In addition to medications, physicians recommend that ulcerative colitis patients make changes in their lifestyle to improve treatment potential and better manage to live with this disease. These lifestyle changes include:
- Reducing stress because less stress may help ease symptoms and prevent more frequent flareups.
- Exercise does not necessarily help patients with ulcerative colitis, but it may help enhance overall health, which can prevent other complications from developing
- A low-fat diet may help reduce the number and severity of flare-ups – especially because higher fat diets are associated with more diarrhea. Physicians may also recommend a diet that is rich in vitamin C as well as one that does not include high levels of fiber because this type of diet may help reduce the frequency of symptoms.
Other medical interventions
If a patient experiences a severe bout of ulcerative colitis, the result can be dehydration, which can lead to the loss of vitamins and electrolytes required to maintain good health. In some cases, poor appetite and severe cases of diarrhea may require that a patient be hospitalized for treatment to restore fluids to the body and make sure that excessive bouts of diarrhea do not cause more serious threats to health.
Surgery
There are many patients who do not respond to any medication and changes to diet do not seem to be helpful. In these cases, surgery may be required in order to effectively treat ulcerative colitis.
In fact, surgery may be considered the only known cure for ulcerative colitis because removing the colon eliminates the possibility of inflammation in that organ. In some cases, surgical intervention may the only option available because holes in the colon, massive blood loss, severe stool blockages, and other complications can be a major threat to health. Two types of the surgical procedure include:
- Proctocolectomy In this procedure, the surgeon will completely remove the entire large intestine, which should remove the inflammation as well. Once the large intestine is completely removed, the surgeon will open a part of the abdomen where the small intestine will empty out into a bag. A patient will need to manage life with a colostomy bag for the rest of their life. Unfortunately, this bag can cause inflammation, too, so another surgical procedure may be another treatment option.
- J-Pouch surgery The other possible surgery is called j-pouch surgery. This type of surgery is similar to the proctocolectomy, but a patient will be able to use the bathroom in a similar way as before the surgery. The diseased part of the colon will be removed, but in this procedure, the small intestine will be tied to an internal pouch which is then attached to the rectum. This will allow the patient to defecate with some normalcy, although bowel movements will be more frequent and watery than usual.
Because surgical intervention is unpleasant at best and can pose risks of complications, the research community has been focusing on another form of treatment – stem cell therapy.
Another treatment option:
Stem cell therapy is based on the body’s natural healing process. As the global scientific community continues to learn more about the nature of inflammatory diseases such as ulcerative colitis, more research is now underway into innovative advancements in cellular medicine – specifically stem cell therapy – as a new approach to treating many different disorders and conditions.
One reason why stem cells are the center of focus for future innovation is that research shows that stem cells have anti-inflammatory properties, which certainly offers promise for inflammatory conditions such as ulcerative colitis. Some research studies indicate that stem cells can signal other cells in the body to balance cytokine production in a way that can help reduce inflammation. That’s why stem cell therapy is now being used to promote the healing of injuries, ease symptoms of rheumatoid arthritis, restore herniated discs in the spine to a more normal shape, and treat many other conditions.
Because stem cells release a number of regenerative and healing factors, they can help promote healing by signaling other cells in the body to regenerate damaged tissues, such as in the colon and rectum – as well as throughout the entire body to help reduce the impact of aging.
Another attribute of stem cells is that they can help the body balance its immune response, which is another factor in the onset and severity of ulcerative colitis.
Research suggests that stem cells create an immunomodulatory effect on T cells, B cells, and NK (natural killer) cells via soluble factors and direct contact with immune system cells. This can prevent the proliferation, maturation, and differentiation of T cells and B cells, which results in fewer white blood cells directed into the colon and rectum, which in turn can reduce inflammation.
Unlike medications often prescribed for ulcerative colitis, stem cell therapy is based on the body’s natural repair processes, so treatment does not usually cause side effects. And compared to surgical procedures, stem cell infusions and injections pose less risk of complications and is widely considered to be a safe treatment.
All of these reasons make stem cells an attractive therapeutic option for patients with ulcerative colitis. Not only can stem cell therapy help reduce inflammation and the severity of flareups, but treatment may also be a way to slow the progression of the disease.
Research insights: How stem cells help treat digestive disorders
Although stem cell therapy can be a successful treatment for many conditions, digestive diseases such as ulcerative colitis demonstrate how stem cells work to ease symptoms and promote healing. Indeed, research into cellular medicine reveals how the body’s natural healing processes work to maintain a healthy digestive system.
These processes can be seen when studying the impact of fasting – not eating food for a period of time – on the natural production of stem cells and how they repair digestive tissue. Some research suggests that a normal routine of eating three meals per day can exacerbate inflammatory bowel diseases and that fasting for a few days at a time (while making sure to drink enough fluids) can boost natural stem cell processes.
Why would fasting help patients with ulcerative colitis? One reason is that digesting food requires energy. When that energy isn’t required for digestion, it can be used to produce stem cells that can heal damaged tissue and restore the immune system functionality required for good health. And because ulcerative colitis may be the result of the immune system misidentifying food as a foreign pathogen, a break from this can help reduce inflammation in the colon and rectum.
One study from the University of California showed that the immune system can completely regenerate itself after just three days of fasting. And researchers at MIT found that in mice, fasting can help regenerate cells. This study compared the intestinal cell production in mice that were not fed for 24 hours with those that were fed normally. The rate of intestinal cell growth in mice that fasted was twice the rate of those that did not fast – demonstrating how this process may be helpful in treating ulcerative colitis.
Another study by the University of California found that mice that had fasted for the equivalent of four days in humans may have actually reversed the pathology of inflammatory digestive disorders. The research suggested that fasting could help the body better regulate microbiota in the digestive system, regenerate cells, and reduce inflammation.
Although these studies on fasting show that stem cell production can help ease symptoms, other researchers are studying treatments that include supplementing the body’s natural supply of stem cells with infusions of new fresh stem cells.
One review of 15 different animal and human studies offers insights into the potential for stem cell therapy as a treatment for ulcerative colitis. This review showed that in mice, stem cell treatment may be helpful in reducing the disease process. An evaluation of several studies in human patients showed the potential for a higher rate of repair of colon and rectal tissue than in patients that did not receive stem cell therapy.
Although these studies are small and additional research is needed to confirm findings, they clearly show the promise of stem cell therapy to alleviate symptoms of ulcerative colitis and delay or even the prevent the need for surgery.
Advanced protocols for screening and culturing high-potency stem cells
While new research into advanced innovative treatments shows exceptional promise in treating frustrating diseases such as ulcerative colitis, it’s important to understand that not all stem cells are alike. Some are more potent than others – and the protocols for testing, processing, screening, and purifying cells at one clinic may not be the same as at another clinic.
At BioXcellerator, we use a specific type of stem cell – mesenchymal stem cells (MSCs) from donated umbilical cords. Research over many years demonstrates that these cells have properties that offer more healing potential than other types of stem cells, such as adult stem cells.
And while using MSCs for treatment may be possible at clinics in the United States, current FDA regulations prohibit reproducing these cells. The difference can result in treatment with only a few thousand cells in the United States, compared to millions of stem cells given to patients treated at clinics outside the U.S.
In addition to considering the number of stem cells provided during treatment, it’s also important to evaluate the protocols the clinic uses to process, test, and purify stem cells to improve the potential for the best possible treatment outcomes. At our lab, which is located at our clinic in Medellin, Colombia, our scientific and medical team has developed an advanced protocol to optimize both the quantity and quality of stem cells given to patients.
This protocol begins with mesenchymal stem cells from donated umbilical cords. Those cells are then screened for specific biomarkers that indicate high potency. Then only those cells that meet our strict criteria are purified and then cultured and expanded into infusions of millions of high-potency stem cells given to patients during treatment.
As for the treatment itself, our medical team customizes a plan based on each patient’s unique needs. In some cases, patients receive stem cells via IV drip. Many of these cells will naturally be transported by the body into the colon and rectum to help promote healing. In other cases, direct injection of stem cells into the colon or rectum may be recommended.
Suffering from ulcerative colitis?
Learn more about advanced stem cell therapy
The BioXcellerator team has worked with many patients who have suffered from ulcerative colitis and has treated many that have reported successful treatment outcomes. Stem cells may not work in every case, but for many patients, it can result in significant improvement.
Our medical team will be happy to consult with you to determine if stem cell therapy may be effective. So if conventional treatment options are not effective, learn more about stem cell therapy – and how it can improve the quality of your life. Simply call 1.888.567.2469 or email Info@bioXcellerator.com to learn more.

