Systemic sclerosis is an autoimmune disease with a large number of symptoms that appear with a range of severities depending on the patient. Some forms of the disease are relatively minor, only affecting the surface of the skin while others will affect the vital organs. The cause of the disease is almost entirely unknown, and current treatment methods are only able to relieve some of the symptoms.
Fortunately, new treatment methods have been devised that use recently developed stem cell technologies to surpass previous treatments and produce better long term outcomes for patients suffering from the disease. First, it may be helpful to understand the disease before jumping into stem cell therapies for systemic sclerosis.
What is Systemic Sclerosis?
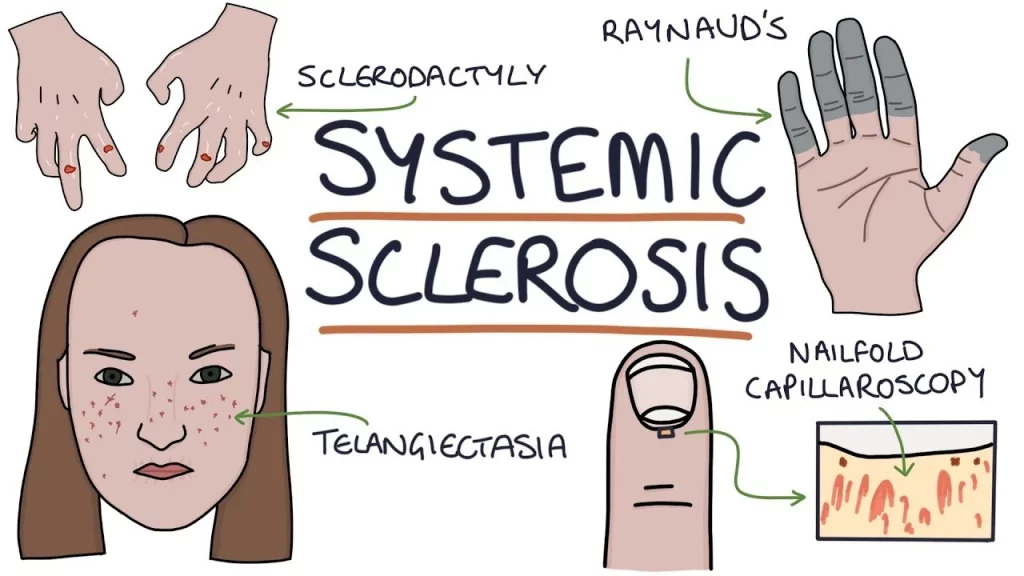
There are a wide range of conditions that fall into the category of “scleroderma”, that affect the connective tissues in the skin, as well as other parts of the body. There are two main forms of scleroderma, known as localized and systemic. Localized scleroderma is limited to affecting only the skin and on occasion some of the nearby tissues. Systemic scleroderma, commonly known as systemic sclerosis, affects tissues throughout the body, including the skin and related tissues, but also the internal organs.
Systemic sclerosis is characterized by an overproduction of collagen. This is a connective tissue found throughout the body and has a variety of purposes related to keeping the structure of various tissues in the correct shape. The overproduction of collagen in different areas causes different symptoms depending on where the excels collagen is found.
Systemic sclerosis presents differently depending on the patient, with the severity and exact nature of the symptoms being experienced varying widely. The main visible symptom is in the skin, which can become red, scaly, flaky, or shiny. Blood vessels are also affected, often becoming constricted or blocked, and appearing more visible. In the limited form, the production is kept mainly to the skin up until the knees or elbows, without affecting the main core of the body. In the diffuse form, excess collagen is also found throughout the entire body, including the internal organs. This form tends to have more severe side effects, since the organs may become unable to function. Both forms may or may not affect the face, depending on the individual patient’s presentation.
As well as the symptoms visible in the skin, those who suffer from the diffuse form of the disease can end up with complications in their organs. If these affect the heart, lungs or kidneys, there can be particularly serious consequences, which can lead to organ failure and death. Less serious, but still problematic, symptoms can occur in the gastrointestinal tract. This can lead to difficulties with digestion or even eating, depending on where the issues occur.
The exact cause of the disease is unknown at the moment. In particular, there is no single genetic cause, although individuals do seem to be more likely to develop the disease if it is present in a family member, so there may be some genetic predisposition. It is suspected that there may be factors that make individuals more at risk of developing the disease, and a particular trigger that determines whether or not an individual will develop the disease. That being said, no specific trigger has been identified so far.
It is not just the cause of the disease which is unknown, the mechanism that leads to the overproduction of collagen that produces the observable symptoms is also currently a mystery. Scientists suspect that the disease is autoimmune. In other words, a malfunction of the body’s own response to damage and infection causes the immune system to attack parts of the healthy body. Autoimmune diseases can be very difficult to treat since it is challenging to find a way to make the immune system correctly identify healthy tissue rather than identifying it as something foreign that needs to be attacked. Moreover, any treatment that suppresses the body’s immune response puts the patient at risk of infection from other pathogens.
Current Treatment Methods
Because so little is known about the cause of the disease and the mechanism through which the symptoms are caused, finding a cure is extremely difficult. Currently there is no single treatment that will cure the disease and eliminate all of the symptoms. Instead, there are a number of different treatments available to try to reduce the severity of the symptoms that are presented, while also slowing down the progression of the disease and maintaining the patient’s quality of life.
The main medical treatments for relieving the symptoms are various medications used to dilate blood vessels, which leads to an increase in blood flow to the extremities to counteract the narrowing of the vessels caused by the disease. Those patients who suffer from gastrointestinal issues may also be prescribed medications to aid with digestion.
The only way to reduce the rate at which the disease progresses is for the patient to take immunosuppressants. This inhibits the body’s natural immune response, which makes the effects of the disease less significant. However, it comes with the extreme downside of putting the patient at a higher risk of contracting an infectious disease. Moreover, immunosuppressants do not prevent the progression, they merely slow it. This therefore puts the patient at higher risk of other disease, while also failing to fully address the problems they face from systemic sclerosis.
Overall, there is clearly much left to be desired in terms of treatments for the disease. Recent advances in our understanding of stem cells have led to new treatments that aim to address the issues faced by those who suffer from systemic sclerosis and will hopefully lead to a cure after further investigation.
Stem Cell Therapy Improves Patient’s Quality Of Life
A number of studies have been carried out in recent years that investigate the benefits of providing individuals who suffer from systemic sclerosis treatment involving transplantation of their own stem cells to try and fight the disease.
Stem cell therapy has seen a number of advances in recent years that allows it to be applied to a wide variety of conditions that were previously untreatable, to improve the quality of life of patients suffering from such diseases, and sometimes to provide a cure.
There are many different forms of stem cell-based treatments that can be used in different situations. Autoimmune diseases tend to be best treated by extracting a patient’s own adult stem cells, processing them suitably and then re-introducing them into the patient where they are needed. Although adult stem cells are less potent than Wharton Jelly stem cells, being able to differentiate into only a few different types of cells, this type of stem cell seems to work for this disease.
For systemic sclerosis, a number of researchers have investigated using autologous hematopoietic stem cell transplants. This is a type of transplant that uses a patient’s own cells, specifically the type of stem cells found in the bone marrow that are responsible for the production of blood cells.
This type of treatment has been known to be safe in humans for many years and has often provided successful new treatment options for a number of different diseases.
For systemic sclerosis, scientists recently published an article that investigated how undergoing autologous hematopoietic stem cell transplants affected the quality of life of patients suffering from systemic sclerosis in the long term. There had already been a number of older studies that showed the effectiveness of the treatment in the short term, but this study was the first to investigate effects of the treatment over a long time period. This is an essential aspect of investigating the usefulness of treatments for chronic diseases like systemic sclerosis, since those that provide relief in the short term but fail to make a difference in the long term are less desirable, and less likely to eventually lead to a cure.
The study looked at over 100 patients in total, comparing patients who underwent autologous hematopoietic stem cell treatment with patients who also suffered from the disease and qualified for the treatment, but did not undergo the treatment. The authors measured the health-related quality of life of the patients, using both the Short Form Health Survey-36 and Health Assessment Questionnaire. The results showed that both one year after the initial treatment, as well as seven years after the treatment, patients who had received autologous hematopoietic stem cell transplants had significantly higher scores than those who received only traditional treatments. Moreover, the difference was larger at the seven year point than the one year point, showing that the treatment actually made a larger difference over time.
This raises a lot of hope for using autologous hematopoietic stem cell transplants as a method of treating systemic sclerosis more widely, and also for refining the treatment to produce more effective results. By finding ways to process the stem cells, or ways to identify which stem cells in particular are making a difference to the quality of life for these patients, researchers may be able to improve the treatments and perhaps produce a cure.
In patients with more severe instances of the disease, more extreme versions of the treatment can be considered. For example, some researchers have investigated the use of myeloablative autologous hematopoietic stem cell transplants, which extracts the stem cells and then uses chemotherapy to kill any remaining hematopoietic cells found in the body and then replaces them with the previously extracted cells.
This procedure is significantly riskier than the usual form of autologous hematopoietic stem cell transplants. The complete eradication of remaining stem cells means that the patient has a greatly reduced immune system until the new transplanted cells take hold, because the hematopoietic stem cells are also those responsible for producing many of the white blood cells that mediate the body’s immune response.
However, for patients who are already at risk from dying from the disease, research suggests that this treatment can be more effective than the conventional therapy. One randomized trial conducted in 2018 compared using myeloablative autologous hematopoietic stem cell transplants with the usual treatment that makes use of the immunosuppressant cyclophosphamide, administered intravenously each month.
Upon analyzing the results, the researchers found that both treatment options had a variety of side effects, including developing infections that could lead to death. However, while the stem cell transplants led to more minor side effects in the short term, it also led to a lower chance that the patients would die from the progression of the disease. It demonstrates that this treatment was more effective in the long term than the traditional administration of cyclophosphamide.
These studies, along with many others, show that hematopoietic stem cell transplants can be used in a variety of ways to help increase the quality of life of patients who are suffering from systemic sclerosis. Additionally, it can treat more aggressive versions of the treatment and can even help to save the lives of those whose disease has progressed to the later stages and puts them at risk of death.
As research continues to progress, new ways to use stem cells to help treat this disease will continue to be developed and refined, to further improve this form of treatment and hopefully save many lives.